1. EEG (Electro Encephalo Graphy)
This is most commonly ordered investigation. It records electrical activity in the brain. Abnormal electrical activity can be recorded in 40-50% children with epilepsy. 4% of normal children may also abnormal electrical activity. Therefore, EEG needs to be interpreted carefully with clinical correlation. Also interpreting pediatric EEGs needs certain amount of expertise and training and therefore better reported by a pediatric neurologist.
EEG is recorded to document the abnormality in the electrical activity and helps in diagnosis and prognosis. EEG is a non-invasive test and does not cause any harm.
Instructions for EEG recording:
1. Hair should be washed before EEG and there should no oil on the head.
2. The child needs to sleep during the test (natural sleep is preferred), therefore he needs to sleep less previous night (sleep withdrawal). He should be made to sleep late at around 12.00 pm and woken up early at 4.00 am. The child should not be allowed to sleep during the travel to EEG lab.
3. No fasting is required. He should have proper meal before the tests.
4. Sedatives which are safe are used to sedate the child if he does not sleep naturally.
2. Video EEG:

A Video EEG test records an EEG and a video at the same time. The purpose is to be able to see the event and compare the EEG records at the same time. Sounds are also recorded.
- Video-EEG This helps to differentiate an epileptic from non-epileptic seizure.
- It helps to record seizure and classify it.
- It helps to pinpoint the region of the brain where seizures begin. Locating the region precisely is essential if epilepsy surgery is being considered.
Video EEG tests can be done at home or in the outpatient setting, like an EEG lab. The duration of tests can vary from 2 hours to 48 hours depending on the need. We often do the test for 2 to 8 hours.
The EEG leads are placed on the child’s head with a special paste, just like routine EEG testing. The head (and electrodes) are usually covered by elastic crape bandage or cap. The electrodes are connected to a wire or cord that is attached to a headbox.
3. Electromyography (EMG):
Electromyography (EMG) is a diagnostic procedure to assess muscles and the nerve cells (motor neurons). Motor neurons transmit electrical signals that cause muscles to contract. An EMG translates these signals into graphs, sounds or numerical values.
EMG results can reveal nerve dysfunction, muscle dysfunction or problems with nerve-to-muscle signal transmission.
EMG results are necessary to help diagnose conditions such as:
- Muscle disorders, such as muscular dystrophy or polymyositis
- Myasthenia Gravis
- Disorders of peripheral nerves – peripheral neuropathies
EMG is a low-risk procedure, and complications are rare.
4. Nerve Conduction Velocity (NCV):
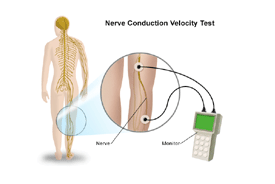
A nerve conduction velocity (NCV) test measures how fast an electrical impulse moves through the nerve. NCV can identify nerve damage. During the test, nerve is stimulated with electrode patches attached to your skin. Two electrodes are placed on the skin over your nerve. One electrode stimulates your nerve with a very mild electrical impulse. The other electrode records it. The resulting electrical activity is recorded by another electrode. This is repeated for each nerve being tested. The speed is then calculated by measuring the distance between electrodes and the time it takes for electrical impulses to travel between electrodes. NCV is required in following conditions in children –
- Guillain-Barre syndrome. A condition in which the body’s immune system attacks part of the peripheral nervous system.
- Charcot-Marie-Tooth disease. An inherited neurological condition that affects both the motor and sensory nerves. It causes weakness of the foot and lower leg muscles.
- Chronic inflammatory polyneuropathy and neuropathy. These are conditions resulting from diabetes or alcoholism. Symptoms may include numbness or tingling in a single nerve or many nerves at the same time.
Nerve conduction studies may also be done to find the cause of symptoms, such as numbness, tingling, and continuous pain.
5. Somatosensory Evoked Potential (SSEP)Test:
It is a test in which we stimulate the nerves in the arm and leg with electrical impulses and record the response from the brain and other parts of the body. The responses are recorded by a computer and the tests interpreted afterwards by a Doctor. It is performed to assess the condition of the nerve pathway. There are no known complications or risks to having an SSEP performed.
6. Visual Evoked Potential (VEP):
A visual evoked potential is an evoked potential caused by a visual stimulus, such as an alternating checkerboard pattern on a computer screen. Responses are recorded from electrodes which are placed on the back of your head and are observed as a reading on an electroencephalogram (EEG). These responses usually originate from the occipital cortex, the area of the brain involved in receiving and interpreting visual signals. The test is useful for detecting optic nerve problems. It measures the time that it takes for a visual stimulus to travel from the eye to the occipital cortex. The test is also useful because it can be used to check vision in children and adults who are unable to read eye charts. A normal VEP can be fairly sensitive in excluding a lesion of the optic nerve, along its pathways in the anterior part of the brain.
- It is a standardized and reproducible test of optic nerve function.
- It is more sensitive compared to magnetic resonance imaging (MRI) in detecting lesions affecting the visual pathway in front of the optic chiasm (area in the optic pathway where the optic nerve crosses sides).
- It is usually less costly compared to other investigations such as MRI.
- If results of the VEP are negative, this can be useful in excluding certain disorders.
7. Otoacoustic emissions (OAE):
Otoacoustic Emission (OAE) Screening is used widely in hospital-based newborn hearing screening programs. Portable OAE screening is the most practical method for screening infants and toddlers.
The procedure is performed with a portable handheld screening unit. A small probe is placed in the child’s ear canal. This probe delivers a low-volume sound stimulus into the ear. The cochlea responds by producing an otoacoustic emission, sometimes described as an “echo,” that travels back through the middle ear to the ear canal and is analyzed by the screening unit. In approximately 30 seconds, the result is displayed on the screening unit as a “pass” or a “refer.”
Otoacoustic emissions (OAE) screening can help to detect sensorineural hearing loss occurring in the cochlea. It can also call attention to hearing disorders affecting the pathway to the inner ear.
Protocol –
1. An initial screening of both ears on every child (at birth)
2. Any ear not passing the initial (1st OAE) screening is screened again (2nd OAE) within approximately 2 weeks of the first screen, if the first screen shows refer.
3. If the ear does not pass the 2nd OAE screen, the child must be evaluated by ENT specialist.
4. If the ear does not pass the OAE rescreen, the child should be referred for further confirmatory tests like BERA.
8. BERA
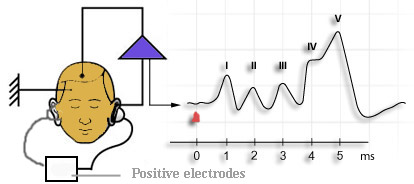
What is BERA test?
The ABR test measures the reaction of the parts of a child’s nervous system that affect hearing. The ABR test measures the auditory nerve’s response to sounds. It performed if a newborn or infant fails the hearing screening test given in the hospital shortly after birth, or for older children if there is a suspicion of hearing loss that was not confirmed through more conventional hearing tests.
- The ABR test is safe and does not hurt.
- The ABR test can be completed only if the child is sleeping or lying perfectly still, relaxed and with his or her eyes closed.
- If your child is younger than 6 months of age, the ABR test usually can be done while he or she naps.
- If your child is older than 7 years, the ABR test usually can be done while your child is awake if he or she can relax and lie still. The test will be done in a special sound-treated suite in the Audiology department.
- For children between the ages of 6 months and 7 years, the ABR test is done under anesthesia, which means that your child will need medication to help him or her sleep throughout the test. ABR tests with anesthesia are done through the Same Day Surgery Center.
- When anesthesia is needed, there are special rules for eating and drinking that must be followed in the hours before the test. If these rules are not followed, the test cannot be done that day.
- When the test is done under anesthesia, your child’s primary care provider will need to see your child for a physical in order to fill out a history and physical form.
- The test itself takes about 1 hour to 11/2 hours, but the entire appointment will take about 2 hours without anesthesia and up to 4 hours if your child needs anesthesia, due to the recovery time.
What Is the ABR Test?
The Auditory Brainstem Response (ABR) test is a helpful tool in determining a child’s ability to hear. The test uses a special computer to measure the way the child’s hearing nerve responds to different sounds.
Three to four small stickers called “electrodes” will be placed on your child’s head and in front of his or her ears and connected to a computer. As sounds are made through the earphones, -the electrodes measure how your child’s hearing nerves respond to them.

The audiologist, or hearing specialist, looks for certain neurological “markers” as your child’s hearing nerves respond to sounds. The softest intensity or loudness level at which these markers appear roughly corresponds to the child’s hearing level in that frequency range or pitch. By reading a computer printout of your child’s responses and interpreting these markers, the audiologist can tell if your child has a hearing problem.
